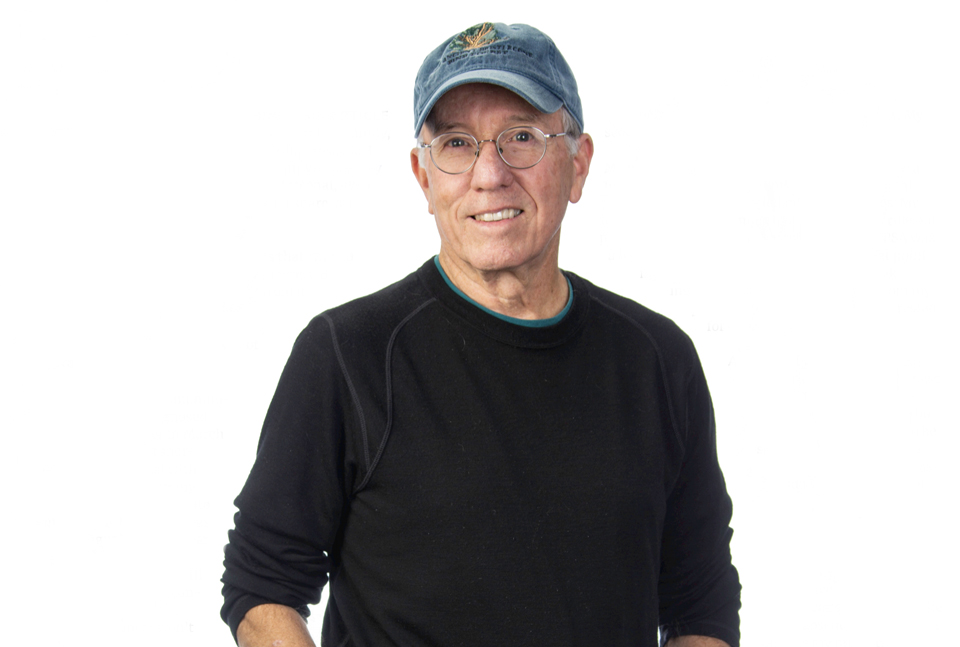
My intention in publishing this article is to be of assistance to any man, and his family, who receives a prostate cancer diagnosis. As I have learned over the last two-and-a-half years, every man’s journey is unique and intensely personal, even though some of the experiences, which I share, are common to all.
The American Cancer Society predicts that 174,650 new cases of prostate cancer will be diagnosed in 2019 and that 31,620 men will die from it. It is the second leading cause of cancer death in American men, behind lung cancer. About 1 man in 41 will die of prostate cancer.
Despite these significant numbers, when I was diagnosed with prostate cancer in March of 2017, and started sharing that information with others, I found that many people did not take prostate cancer seriously, as if it was “cancer light.” I would hear comments like, “Any man who lives long enough will probably get prostate cancer,” or, “Most men who get prostate cancer won’t die from it.”
While there is some truth in both statements, I can assure anyone who has not had cancer that there is no such thing as cancer light, and that what seems like a cultural misunderstanding of prostate cancer minimizes the life changing consequences of its diagnosis and disrespects the men, and their families, who are coping with it. Prostate cancer is a serious disease.
As a preliminary to a routine physical in December 2016, age 68, I had a Prostate Specific Antigen (PSA) test, the results of which can be an indicator of the presence of prostate cancer. Any score above 4.0 is cause for concern, as are scores that double over a reasonably short time; for example, from a 1.7 to a 3.4. My score was a 7.1.
My primary care doctor recommended that I see a urologist. I had no symptoms and a digital rectal examination (DRE) revealed no abnormalities. My urologist put me on a month of antibiotics to rule out prostate inflammation or infection. My next PSA was a 6.9, as was a follow-up a week later. At that point my urologist recommended a biopsy, taking twelve random core samples from my prostate gland and having them tested for cancer.
A prostate biopsy is an unpleasant experience, but it is the best way to determine the presence of cancer. I had mine on March 15, 2017. I received the shoulder slumping results on March 22nd: cancer was found in ten out of twelve tissue samples. I had prostate cancer. My Gleason score was a 6, which indicated that my cancer was mildly to moderately aggressive. Bone and soft tissue scans determined the likely absence of any cancer outside my prostate, which was good news.
Cancer does not go away by itself. Once you know you have cancer it lodges in your brain and psyche, and it influences how you think and feel about your life. The next step for me was to decide what treatment plan I wanted to follow. One was to do nothing. Some men choose that option and end up dying as a result. Another option was active surveillance, also known as watchful waiting, which includes regular PSA tests, internal exams and another biopsy at some point, usually within a year. More dramatic treatments include surgery to remove the prostate cancer or radiation to target, as much as possible, and kill the cancer in the prostate.
Because I was otherwise active and healthy, and my Gleason score wasn’t in the aggressive 7 to 9 range, I chose active surveillance and proceeded to learn as much as I could about prostate cancer and how it is perceived in the lay and medical world. I had time to do research and be prepared to make an informed decision if tests showed that my cancer was getting more aggressive.
For nine months my PSA stayed in the high 6 to low 7 range. I joined a support group at the Hearst Cancer Resource Center at French Hospital and began to understand how personal and varied each man’s journey with prostate cancer can be. The group is a wonderful resource and I highly recommend it, for both information and emotional support, to any man who has been diagnosed with prostate cancer. I also learned about the potential side effects of both surgery and radiation.
The two most common side effects of aggressive treatment for prostate cancer are incontinence and erectile dysfunction due to damage done to nerves and muscles integral to both. They can be short term, long term or permanent. No man would welcome the possibility of either of those conditions if he could avoid them. Unless his life is in danger or because the psychological burden of walking around with cancer becomes too heavy.
In January 2018 my PSA went up to 8.3. Given what I had learned over the previous ten months, and the shared experience of individuals in my support group, I began to think it was time for more aggressive treatment. I was also influenced by friends and family who were concerned about the possibility of the cancer getting more aggressive and spreading. I seriously considered two types of radiation: photon and proton; and surgery: a radical laparoscopic prostatectomy.
Photon radiation was available locally and required roughly 35 outpatient treatments over seven weeks. Proton was only available in Loma Linda or San Diego and required living there during the treatment. The surgery required one night at Sierra Vista Hospital where there is a Da Vinci robot. Radiation reduces the possibility of side effects, but it gets complicated if not all of the cancer is removed or if it returns. Surgery virtually guarantees the side effects but reduces concerns about not getting all of the cancer by completing removing the prostate.
I was leaning toward proton radiation, which causes less collateral damage than photon, when one day, while walking my dog, I had a sudden insight: stay close to home where you have the most support; trust your doctor who has performed a thousand robotic surgeries; get this over with and start your recovery as soon as possible. I made an appointment with my doctor at the end of February and told him I wanted to have surgery. After almost a year of walking around with cancer, it was a relief to make a decision.
I had my surgery on April 16, 2018, and I was home the next day. The first few days were difficult. I had five incisions, I was bloated and in a lot of pain, and I had a catheter. I wouldn’t want to relive those days. But with gradual improvement, getting on my feet and walking as soon as possible, I started feeling better. As she had since my diagnosis, my wife, Melinda, gave me tremendous support, as did my friends and family. My first PSA test, 30 days after my surgery, indicated that I was cancer free, as have subsequent tests.
I hoped I would be the exception to the rule regarding side effects, but that wasn’t the case. With natural healing, exercises and some physical therapy, I have experienced steady improvement. Within a couple of months I was back to my preferred physical activities: hiking, rock and indoor climbing, playing golf. In September Melinda and I did a twelve-mile round trip hike in the Eastern Sierra to Bishop Pass, just under 12,000’, and in January we spent eight days on Kauai, hiking, snorkeling and celebrating her recent retirement.
I have had some difficult, demoralizing days in the last couple of years, but today I consider myself fortunate. The disease was detected before it spread, the surgery seems to have eliminated the cancer, my lifestyle has not been radically altered, and I have a greater overall appreciation for the quality of my life and the loved ones who have been with me on this journey. And for the sake of all those whose lives might be impacted by prostate cancer, I repeat: There is no such thing as cancer light.
For more details about my experience, you can read my articles published by ProstateCancer.net, a free interactive website that also has a FaceBook page, or you can contact me at willnlf@charter.net
On Pacific Time.
Always open.
Email or call
805-466-2585
Loving Life on the
Central Coast, California
On Pacific time.
Always open.
Email or call
805-466-2585